Abstract
Background: Acute myeloid leukemia (AML) secondary to haematological neoplasia or other malignant diseases, defined as secondary AML (sAML), is thought to have an inferior prognosis as compared with de novo AML. However, when corrected for other risk factors such as age and cytogenetic risk, differences are less clear. In particular, it is uncertain whether outcome after allogeneic stem cell transplantation (alloSCT) is different. Thus, the Acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT) performed a registry-based analysis to compare results after alloSCT for sAML versus de novo AML.
Methods: Inclusion criteria were age >= 18y and alloSCT for de novo or sAML from a matched related, matched unrelated or T-cell replete haploidentical donor between 2000 and 2016. Patients without information on cytogenetics were excluded. 11439 patients with de novo and 1325 with sAML were identified. A multivariate Cox model was performed to account for imbalances of risk factors between the two cohorts; it was stratified for different stages at alloSCT, due to a significant interaction between stage at transplant and diagnosis (de novo or secondary) . In a second approach, a matched pair analysis of secondary versus de novo AML was done, using the following criteria for matching: Age (+/-3 years), stage at alloSCT, Karnofsky performance score, conditioning intensity, in and ex vivo T cell depletion, donor type, donor/recipient sex and CMV-status combination, cytogenetics, and graft source.
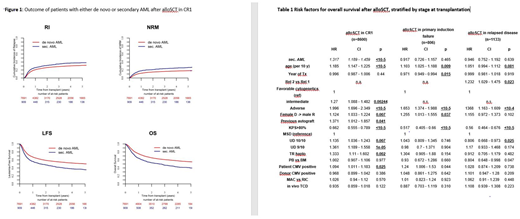
Results: Median follow up after alloSCT was 36 and 33 months for de novo and sAML, respectively. In a multivariate Cox model focusing on transplants in first complete remission (CR1), sAML was associated with a higher non-relapse mortality (NRM; HR=1.32; p<10-5) and relapse incidence (HR=1.28; p=0.0002), and a lower leukemia-free survival (LFS, HR=1.30;, p<10-5), overall survival (OS, HR=1.32; p<10-5 ) and GvHD/relapse free survival (GRFS, HR=1.20; p<10-5 ), as compared to de novo AML. Other prognostic factors for OS were age (p=<10-5), cytogenetics (intermediate, p=0.002, poor, p=<10-5), patient/donor sex combination (female in male, p=<10-5) KPS (<>80, p=0.003) and donor type (unrelated (UD) 10/10 match, p=0.007; UD 9/10 match, p=10-5; haplo, p=0.002)., Three-year cumulative incidence of relapse and non-relapse mortality after alloSCT in CR1 were 28.5%/16.4% for de novo AML (n=7691), and 35%/23.4% for sAML (n=909), 3-year overall survival (OS), leukemia-free survival (LFS) and GvHD-relapse-free survival (GRFS) were 60.8%, 55.1% and 38.6%for de novo and 46.7%, 41.6% and 28.4% for sAML. (Figure 1). In contrast, when focusing on patients transplanted for primary refractory disease (sAML, n=199, de novo AML, n=607) or for relapsed leukemia (sAML, n=124, de novo AML, n=1009), Cox models did not identify sAML as a relevant factor for outcome. Risk factors for OS in advanced disease stages are presented in Table 1.
Using the criteria described above, 877 well-matched pairs were identified. The pair-matched analysis confirmed the above findings: Over all patients, sAML was associated with higher NRM (p=0.004) and lower LFS (p=0.004), OS (p=0.008) and GRFS (0.04). However, when the analysis was stratified by stage at SCT, again differences were only seen among patients transplanted in CR1 (719 pairs, 82%), but not after alloSCT in advanced disease.
Conclusion: Our large-scale, registry-based analysis identified sAML as an independent risk factor for outcome after alloSCT in first complete remission. In primary refractory and relapsed AML, other factors such as age, cytogenetics and performance status were of higher relevance. This data may help to improve risk stratification and prognostic estimates after alloSCT for sAML.
Schmid:Jazz Pharma: Honoraria, Other: Travel grant, Speakers Bureau. Ganser:Novartis: Membership on an entity's Board of Directors or advisory committees. Beelen:Medac: Consultancy, Other: Travel Support. Mohty:MaaT Pharma: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal